Dementia Diagnosis
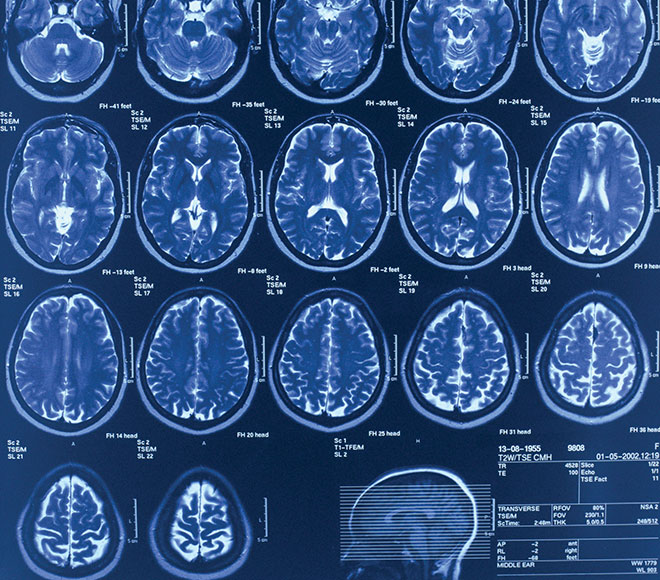
Diagnostic Criteria
The Alzheimer's Association and the National Institute on Aging (NIA) jointly issued four criteria and guidelines to diagnose Alzheimer's disease, including recommendations for clinical office settings.

Access resources for your patients and their caregivers.
See Resources
Assessment and care planning services now eligible for reimbursement.
Learn More



