Triple Your Impact This Holiday Season
Triple Your Impact This Holiday Season
Celebrate the holidays with a year-end gift that can go 3x as far to help provide care and support to the millions affected by Alzheimer's disease, and to advance critical research. But please hurry — this 3x Match Challenge ends soon.
Donate NowTraumatic Brain Injury (TBI)
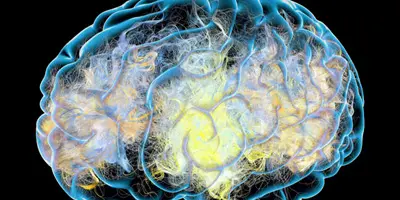
Traumatic brain injury (TBI) results from an impact to the head that disrupts normal brain function. TBI may affect a person's cognitive abilities, including learning and thinking skills.
About traumatic brain injury
 Most TBIs are caused by falls, being struck by an object or by vehicle crashes. Doctors may classify traumatic brain injury as mild, moderate or severe, depending on whether the injury causes unconsciousness, how long unconsciousness lasts and the severity of the individual's symptoms. Although most TBIs are classified as mild because they're not life-threatening, a mild TBI can have serious and long-lasting effects; the extent of these effects is not fully understood and requires more research.
Most TBIs are caused by falls, being struck by an object or by vehicle crashes. Doctors may classify traumatic brain injury as mild, moderate or severe, depending on whether the injury causes unconsciousness, how long unconsciousness lasts and the severity of the individual's symptoms. Although most TBIs are classified as mild because they're not life-threatening, a mild TBI can have serious and long-lasting effects; the extent of these effects is not fully understood and requires more research.
Some of these injuries are considered primary — damage and symptoms are immediate. Other outcomes of TBI can be secondary — they can occur gradually over hours or days, or appear weeks later. These secondary brain injuries are the result of reactive processes that occur after the initial head trauma.
TBI resulting from an impact to the head disrupts normal brain function and is a threat to cognitive health in two ways:
- A traumatic brain injury's direct effects — which may be long-lasting or even permanent — can include unconsciousness, inability to recall the traumatic event, depression, confusion, difficulty learning and remembering new information, trouble speaking coherently, unsteadiness, lack of coordination and problems with vision or hearing.
- Certain types of TBI may increase the risk of developing Alzheimer's or another type of dementia years after the injury takes place.
If a head injury occurs
TBI can affect your brain even if you don't lose consciousness and your symptoms clear up quickly. Anyone who experiences an impact to the head and develops any symptoms of TBI should seek medical attention, even if symptoms seem mild. Call emergency services for anyone who:
- Is unconscious for more than a minute or two. Experiences seizures, repeated vomiting or symptoms that seem to worsen as time passes.
- Was ejected from a vehicle and sustained a head injury.
- Was struck by a vehicle while on foot.
- Has fallen from a height of more than three feet.
Causes and risk factors
The leading causes of TBI that result in emergency department visits are falls, being struck by an object and motor vehicle crashes. Indirect forces that shake the brain violently within the skull, such as shock waves from battlefield explosions, can also cause TBI. In addition, TBI can result from bullet wounds or other injuries that penetrate the skull and brain. However, it is important to note that not all blows or jolts to the head result in a TBI.
Falls are the most common cause of TBI, and falling poses an especially serious risk for older adults. According to the CDC, approximately 1 in 4 Americans ages 65 and over reports falling each year. Falls lead to 3 million emergency department visits per year. The number of deaths from falls is rising. Between 2007 and 2016, the number of deaths among older Americans rose 62%, to 29,668. Those ages 75 and older are three times as likely as those between 65 and 74 to be hospitalized from a fall. Men are twice as likely to be hospitalized as women.
When a person over 65 years old sustains a serious TBI in a fall, direct effects of the injury may result in long-term cognitive changes, reduced ability to function and changes in emotional health. Older adults who experienced loss of consciousness after a TBI were 28% more likely to report subjective memory impairment than seniors who did not experience a TBI.
Preventing traumatic brain injury
Measures to reduce the risk of falls include:
- Using a walker or other assistive device to compensate for mobility problems, muscle weakness or poor balance.
- Having your vision checked regularly and using glasses or contact lenses that correct for changes.
- Working with your doctor to watch for medication side effects or interactions among drugs you're taking.
- Avoiding household hazards, such as clutter, loose rugs or bad lighting.
- Protecting your head by wearing a helmet and other protective equipment when biking, inline skating or playing contact sports.
- Keeping your vehicle in good repair, following the rules of the road and buckling your seat belt.
Home safety and dementia
Use our online tool, ALZNavigator™, and get a personalized action list on how to prevent falls and make your home safe for someone with dementia.
Symptoms
The severity of symptoms depends on whether the injury is mild, moderate or severe. In all forms of TBI, cognitive changes (changes in how people think) are among the most common, most disabling and longest-lasting symptoms that can result from the injury. The ability to learn and remember new information is often affected. Other commonly affected cognitive skills include the capacity to pay attention, organize thoughts, plan effective strategies for completing tasks and activities and make good judgments. More severe changes in thinking skills — a hallmark characteristic of dementia — may develop years after the injury took place and the person appears to have recovered from its immediate effects.
Symptoms of mild TBI
Mild TBI, also known as a concussion, does not necessarily cause loss of consciousness or causes unconsciousness that lasts for 30 minutes or less. Mild TBI symptoms may include:
- Inability to remember the cause of the injury or events that occurred immediately before or up to 24 hours after it happened.
- Confusion and disorientation.
- Difficulty remembering new information.
- Problems with finding words.
- Headache.
- Dizziness.
- Blurry vision.
- Sensitivity to light and/or sound.
- Change in energy or motivation.
- Nausea and vomiting.
- Ringing in the ears.
- Trouble speaking clearly.
- Changes in emotions or sleep patterns.
These symptoms usually appear at the time of the injury or soon after, but sometimes may not develop for days or weeks. Mild TBI symptoms are usually temporary and clear up within hours, days or weeks; however, on occasion, they can last months or longer.
Symptoms of moderate and severe TBI
Moderate TBI causes unconsciousness lasting more than 30 minutes but less than 24 hours, and severe TBI causes unconsciousness for more than 24 hours. Symptoms of moderate and severe TBI are similar to those of mild TBI, but more serious and longer-lasting. The more severe injuries may also lead to hemorrhages or other brain injuries that are associated with focal neurologic symptoms, such as localized weakness or sensory loss.Diagnosis
Evaluations by health care professionals typically include:
- Questions about how the injury happened.
- Assessment of the person's level of consciousness and confusion.
- An examination to assess memory and thinking, vision, hearing, touch, balance, gait, coordination, strength and sensation, reflexes and other indicators of brain function.
Let your physician know if you are taking medications (prescription, over-the-counter or natural remedies), especially blood thinners such as Coumadin and aspirin, because they can increase the chance of complications. Also inform your health care professional if you drink alcohol or take drugs.
Depending on the cause of the TBI and the severity of symptoms, brain imaging with computed tomography (CT) or magnetic resonance imaging (RN) may be needed to determine if there's bleeding or swelling in the brain. If you experience a TBI, it should be noted in your permanent medical record and mentioned whenever giving a new doctor your medical history.
Does every hit to the head lead to dementia?
There's no evidence that a single mild TBI increases cognitive decline and dementia risk. Although currently, there's no known strategy to reduce the possible long-term risk of cognitive decline and dementia once you've experienced a moderate or severe TBI or repeated mild traumatic brain injuries, it's important to understand that not everyone who experiences a head injury in one of these categories develops dementia. Ongoing research is aimed at understanding the underlying mechanisms of the connection between TBI, cognitive decline and dementia in the brain, including the role of potential exacerbating factors.
Treatment
The most serious traumatic brain injuries require specialized hospital care and can require months of inpatient rehabilitation. Most traumatic brain injuries are mild, however, and can be managed with either an ER visit, a short hospital stay for observation or at-home monitoring followed by outpatient rehabilitation, if needed.
Treatment of dementia in a person with a history of traumatic brain injuries varies depending on the type of dementia diagnosed. Strategies for treating Alzheimer's or another specific type of dementia are the same for individuals with and without a history of TBI.
However, the contributions of TBI to cognition is a relatively new area of exploration for researchers and physicians, formal clinical guidelines for diagnosing and managing this condition do not yet exist. Several major research initiatives are under way to gain further insights into the patterns of injury and brain changes implicated in the context of TBI, and to develop new strategies for prevention, diagnosis and treatment.
Learn more: Treatment for Dementia, Treatment for Alzheimer's
Dementia help and support are available
The Alzheimer's Association can help you learn more about Alzheimer's and other dementias, and help you find local support services. Call our 24/7 Helpline at 800.272.3900.
Brain Injury Association of America (BIA) is an education, advocacy and research organization that offers support to people with brain injuries and their families. Call their information center at 800.444.6443.
Centers for Disease Control (CDC) has a traumatic brain injury section that offers information about research studies and prevention and education programs.
The Concussion Legacy Foundation provides chronic traumatic encephalopathy (CTE) information and resources.
Supporting traumatic brain injury research, the National Institute of Neurological Disorders and Stroke (NINDS) has a traumatic brain injury section that offers information about treatment, clinical trials and resources.
Research on cognitive decline, dementia and traumatic brain injury
Over the past 30 years, research has linked moderate and severe TBI to a greater risk of cognitive decline or dementia years after the original head injury. The key studies showing an increased risk found that older adults with a history of moderate TBI had a 2.3 times greater risk of developing Alzheimer's than seniors with no history of head injury. Those with a history of severe TBI had a 4.5 times greater risk. Other studies — but not all — have found a link between moderate and severe TBI and higher risk of cognitive decline and dementia.
- There's no evidence that a single mild TBI increases dementia risk. However, emerging evidence does suggest that repeated mild traumatic brain injuries, such as those that can occur in sports like American football, boxing, hockey and soccer, may be linked to a greater risk of traumatic encephalopathy syndrome (TES) or specific brain changes associated with chronic traumatic encephalopathy (CTE).
- The symptoms of TES/CTE may include memory loss, confusion, impaired judgment, impulse control problems, aggression, depression, anxiety, suicidality, parkinsonism (movement symptoms similar to Parkinson's disease) and, eventually, progressive dementia. These symptoms may begin years or even decades after the last traumatic brain injury.
- Previous research has shown that boxers have an increased risk of specific brain changes associated with CTE and may be associated with changes in cognition. When an individual had these memory changes in the context of boxing-related injury, this was originally called dementia pugilistica or "punch-drunk syndrome." The risk of the specific brain changes associated with CTE in boxers seems most closely tied to the number of rounds boxed, not to the number of times a boxer was knocked out, suggesting that even repeated mild traumatic brain injuries that don't cause unconsciousness may increase dementia risk. Brain changes associated with CTE can occur following a small number of severe traumatic brain injuries, or a large number of mild or very mild traumatic brain injuries, or some other pattern of head trauma.
- In a study published in the March 23, 2016, online edition of the Journal of Neurology, Wei Li and colleagues found that a history of TBI may accelerate the age of onset of cognitive impairment by two or more years. These results were consistent with other studies that indicate TBI is a significant risk factor for cognitive decline in older adults and associated with an earlier age of onset in people with mild cognitive impairment and Alzheimer's disease.
- Another study conducted by researchers at Umeå University in Sweden also found that TBI is a risk factor for dementia and revealed that the risk of a dementia diagnosis was highest during the first year after the injury. During this time, people who had a TBI were four to six times as likely to get a dementia diagnosis as those without a TBI. The study also concluded that a concussion or other TBI can increase the risk of developing dementia even 30 years later.
- A study published in 2021 in GeroScience demonstrated that brain changes in people with mild TBI and Alzheimer's had similarities. The researchers found that there was a reduction in cortical thickness in both Alzheimer's and TBI individuals when compared to healthy individuals. Cortical thinning is often associated with reduction in memory, verbal fluency and integrating new information and with decreased ability to make decisions
- More research is needed to fully understand the relationship between TBI and dementia and to understand why moderate, severe and repeated mild traumatic brain injuries are at an increased risk with changes in memory, thinking and reasoning in individuals in later life.
- Traumatic brain injury may be more likely to increase the risk of dementia in individuals who have a specific variant of the gene for apolipoprotein E (APOE) called APOE-e4. More research is needed to understand the strength of the link between APOE-e4 and dementia risk in those who've had a TBI.
Related Pages

The Alzheimer’s Association is in your community.
Find Your Local Chapter
Learn how Alzheimer’s disease affects the brain.
Take the Brain Tour